Macular disease
The macula refers to the most central part of the retina,
and the other part of retina is called peripheral retina relative to the macula area.
In fact, the macular disease is a general term for many possible diseases.
The following four are very common and mostly treatable diseases:
Age-related macular degeneration
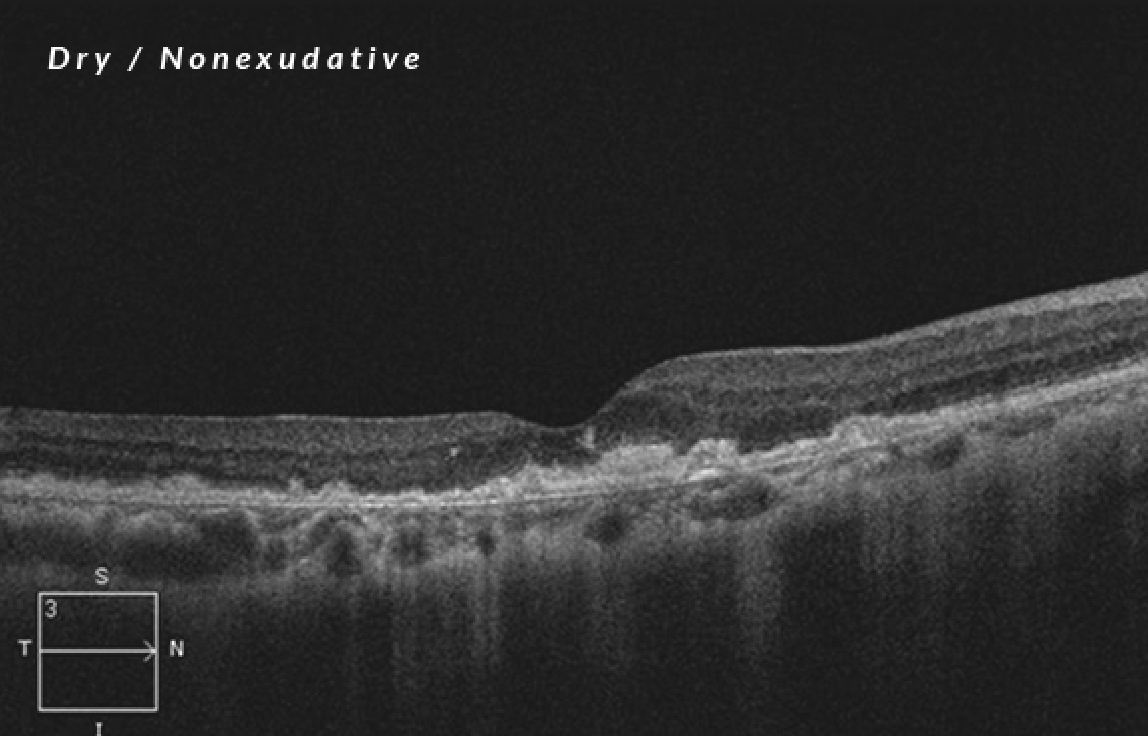
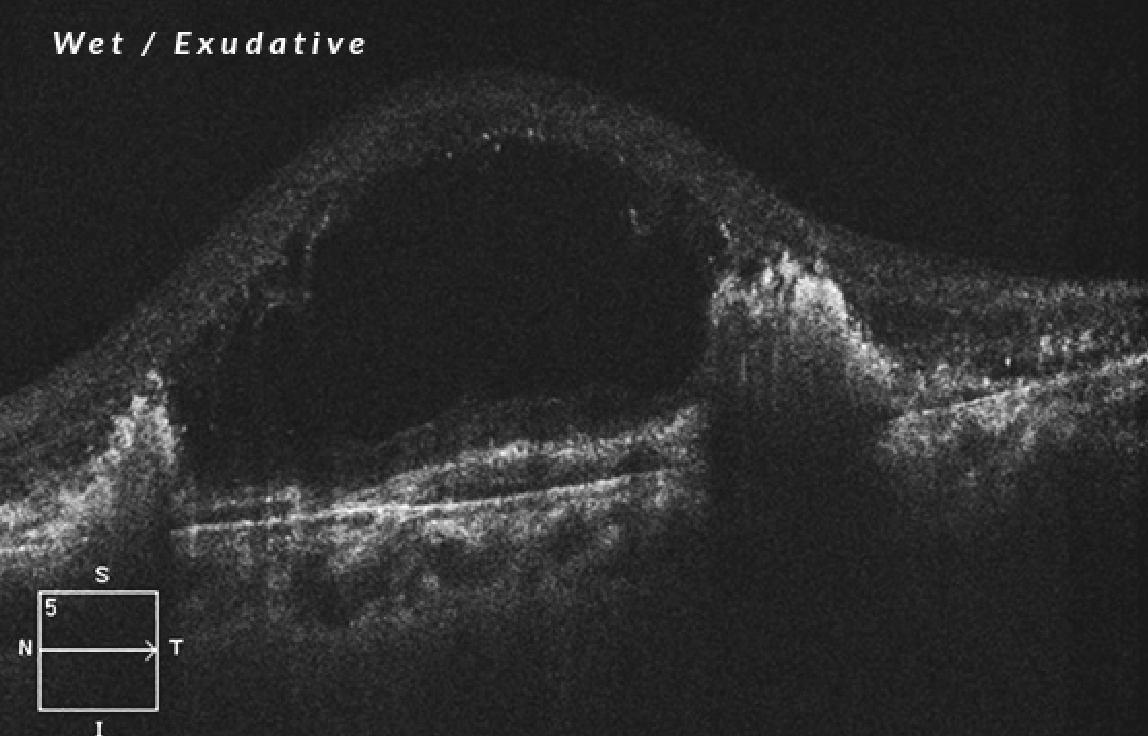
Depending on the presence of choroidal neovascularization, age-related macular degeneration is divided into two types: dry/nonexudative and wet/exudative.
Nonexudative type results from retinal cell atrophy and scarring. There is no choroidal neovascularization, and usually it has a minor effect on visual acuity with slower progression. Once it becomes exudative, it means that neovascularization has formed in the choroid behind the retina, which would leak exudates and fluids and also cause hemorrhage, and that will lower the visual acuity in severe cases.
Symptoms
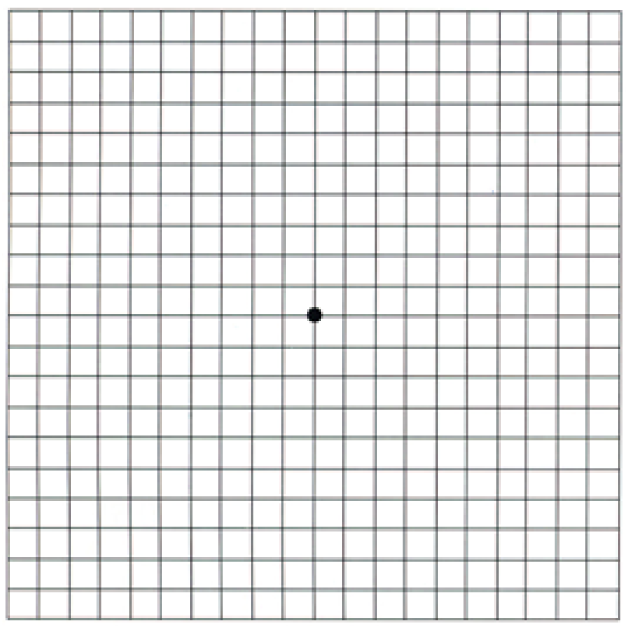
Amsler Grid
Steps:
1. Put this table 30 cm in front of you.
2. If you have presbyopia or myopia, you need to wear appropriate glasses.
3. Cover one of your eyes with one hand and use the other eye to gaze at black spot at the center of the table.
4. You can only focus your eye on the black spot without looking at the lines next to them.
5. “Feel” the lines and see if there are any distortions, dark shadows, or blurred places.
The treatment of age-related
macular degeneration
If it is a dry type, treatment is hard, but it is still necessary to have regular checks at an ophthalmology clinic, and the ophthalmologist will evaluate whether it is converted into a wet lesion. Now, the most effective treatment for exudative age-related macular degeneration is the anti-VEGF injection therapy, which directly injects the drug into the vitreous of the eye.
The most common medicines are Avastin, Lucentis and Eylea, and the latter two are more effective. The patient meeting some requirements can be reimbursed by national health insurance, and save tens of thousands of fees. Other treatments include low-energy laser treatment, which is used only on neovascularization lesions that are farther from the center of the macula; photodynamic therapy, which combinesintravenous light-sensitive drugs with laser treatment, selectively destroys neovascularization, but reserves normal.
Prevention of age-related
macular degeneration
Age-related macular degeneration factors include chiefly age, then genes, smoking, high cholesterol, obesity, overexposure to ultraviolet radiation, high blood pressure and arteriosclerosis. Therefore, what is important is not smoking, keeping healthy, having good daily life habits, and wearing UV-protection sunglasses outdoors. Secondly, healthy foods with vitamins C, E, zinc oxide, lutein, and zeaxanthin can reduce the occurrence or deterioration of age-related macular degeneration.If you find the signs and symptoms of the above-mentioned macular degeneration, you had better consult a professional ophthalmologist for possible medical treatments as soon as possible.
Diabetic macular edema
-
The causes of diabetic macular edema
Type 1 diabetes is a condition in which a body cano not produceenough insulin. Type 2 diabetes arises for insulin-resistant factors. Both cause high blood sugar and will lead to diabetic retinopathy after having high blood sugar level for a long time.
-
The symptoms
Almost type 1 diabetes patients will have diabetic retinopathy 15-20 years later, and 20%-30% of them will be blind; type 2 diabetes patients will have diabetic retinopathy about 20 years later. A quarter of the patients with diabetic retinopathy will have diabetic macular edema 15 years later.
-
The treatment
Diabetic retinopathy, like diabetes, cannot be fully cured, but appropriate treatments can restore vision and alleviate the illness. In general, it’s fine to track non-proliferative retinopathy ; proliferative retinopathy needs laser treatment or vitrectomy. If macular edema occurs, just like exudative age-related macular degeneration, vision can often improve greatly after the anti-VEGF injection therapy.
Epiretinal membrane on macula
The causes
The epiretinal membrane (ERM), a membrane that does not belong to any normal tissue covers the retina. The most common cause is spontaneous. It is related to a phenomenon called "posterior hyaloid detachment," which starts with the physiological liquefaction of the vitreous, then the solid part moves forward. Other factors include inflammation in the eyeball, traumas, retinal vasculopathy, retinal tears, and retinal surgery.
The symptoms
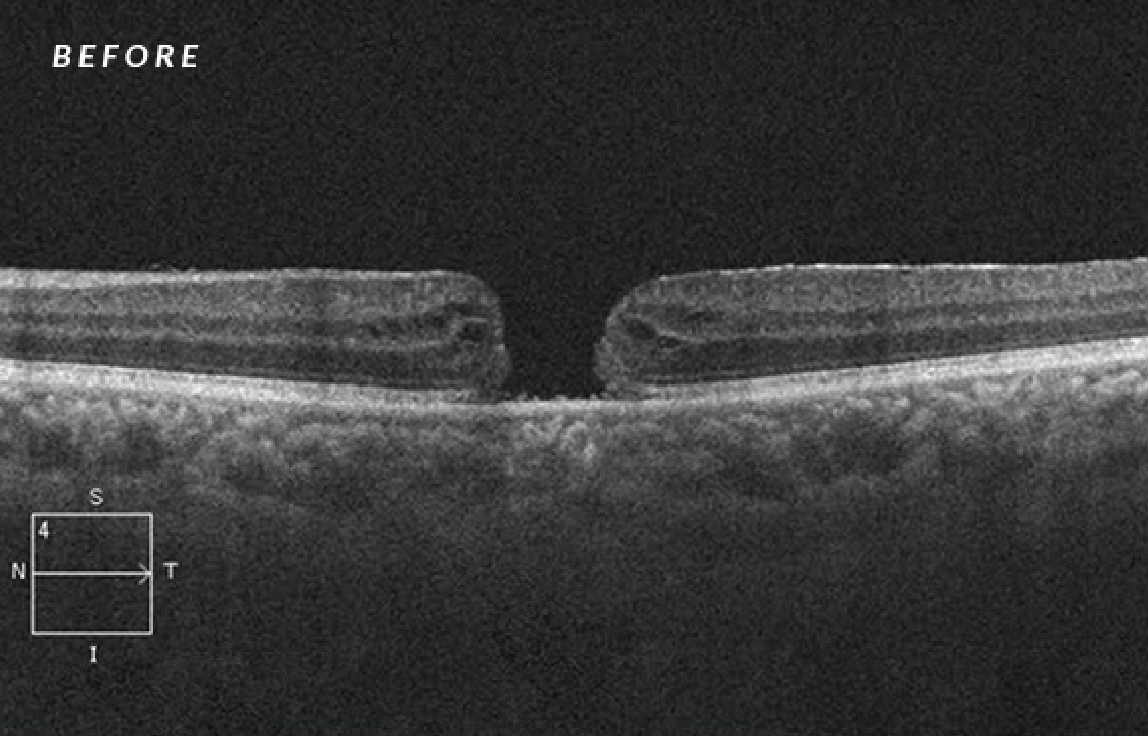
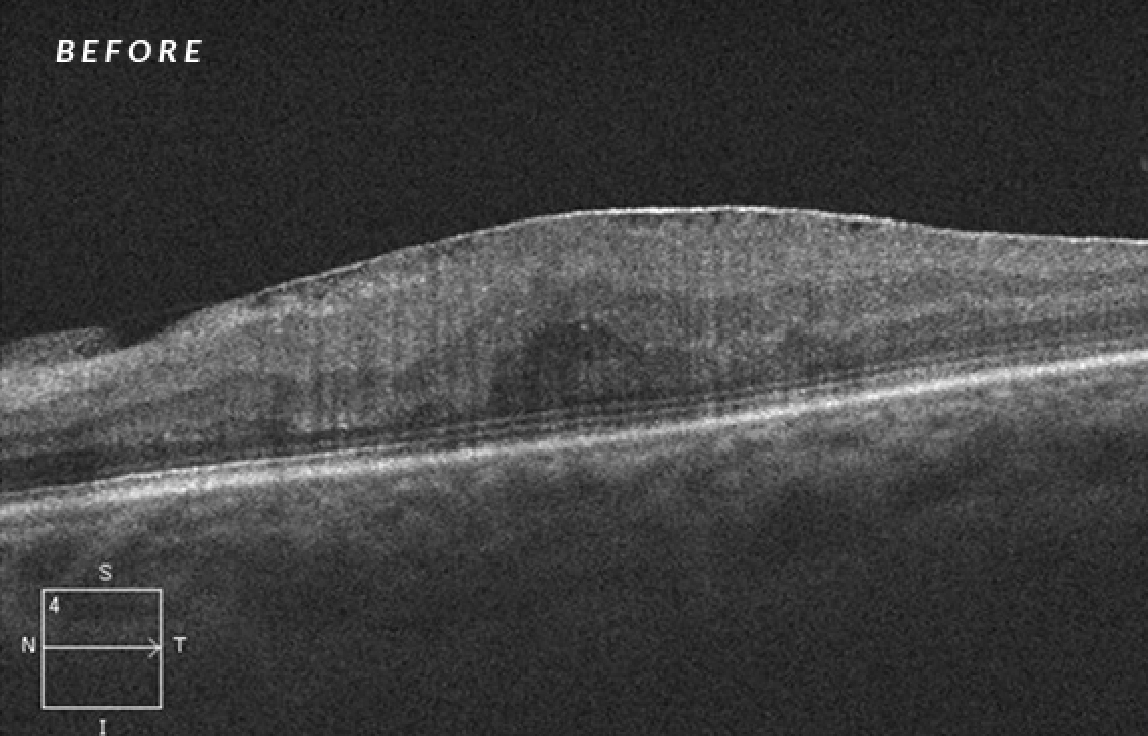
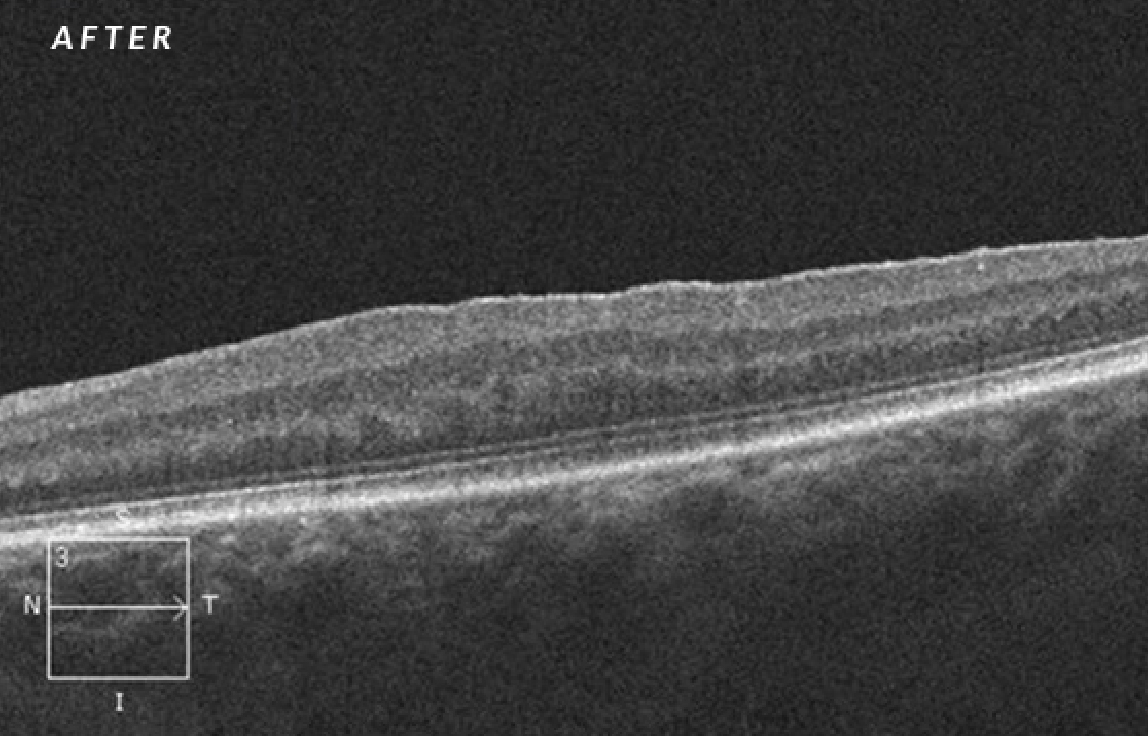
The epiretinal membrane on macula cause wrinkles, and the distorted macula would lead to distorted vision, sometimes with decreased visual acuity, and enlarged objects in the affected eye. You can do a simple test by yourself with the Amsler grid.The optical coherence tomography(OCT) can make a precise diagnosis. It can clearly show an abnormal hyperplasia membrane in the macular section.
The treatment
Epiretinal membrane removal surgery.
The progression of the epiretinal membrane is slow, so the disease is mainly observed at the beginning. When the epiretinal membrane on the retina continues to deteriorate, seriously affecting the visual quality, or causing complications of the macular hole, surgery can be considered to improve vision.
The macula is very sensitive, and is responsible for almost all the front vision. Actually retina is a thin, membrane-like tissue, and we need to tear epiretinal membrane, another thinner and almost invisible membraneattached on the membrane-like tissue, so it is a very rigorous and meticulous microsurgery, which bears no error. Usually, after peeling off the epiretinal membrane on the retina, it is necessary to remove a small piece of the uppermost tissue on the retina—internal limiting membrane (ILM).
This procedure does not affect vision, but can greatly reduce the chance of recurrence of the epiretinal membrane.It usually takes several months for the damaged nerve fiber and photoreceptor cells to recover. Therefore, visual acuity sometimes improves after a few months after surgery. The postoperative care is also very important.
Macular hole
The causes
Almost all the front vision is taken charge of by the macula. At the center of the macula is . The fovea is an area with highly concentrated photoreceptor cells, providing detailed vision and color discrimination at the center of the front visual field. The image on the fovea helps let the eyes to focus objects, so people would unconsciously align the things they want to see at the center of vision. The macular hole refers to the broken retina in the macula area, mostly just in the fovea, thus greatly affecting the visual acuity.
The most common cause is spontaneous. Other risk factors include vitreous traction, epiretinal membrane, high myopia, contusion, inflammation in the eyeball, and diabetes.
The symptoms
The treatments
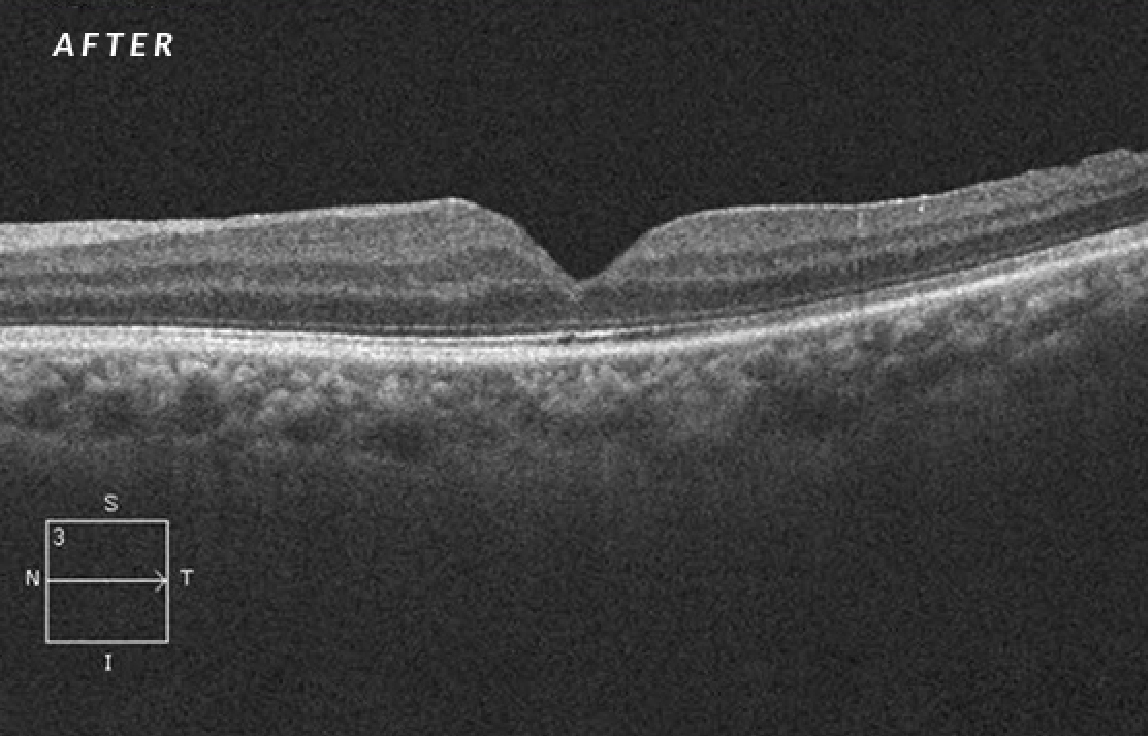
There are four stages of the macular hole. In the treatments, the patients with the holes less than 250 μm in size of stage 1 and stage 2 may consider intraocular injection of recombinant microplasmin (Ocriplasmin) to heal the holes; the patients with the holes more than 250 μm in size of stage 3 and 4 are mainly treated with surgery.
The purpose of the surgical treatment is to release the tension around the macular hole, and then use gas to push back and close the hole. If the hole is too large, removal of the internal limiting membrane (ILM) can release more tension and enhance the healing opportunity. If central retinal detachment is combined, more stable silicone oil than air can be used instead to increase the success rate of surgery.
Usually, the fissure will heal within one month after surgery, but it still takes several months to several years for the nerve fibers and photoreceptor cells under the original site of the hole to grow and recover. Therefore, although the central blind spot will gradually become lighter from black, it still takes a while for the resolution to be improved.
Compared with the epiretinal membrane, the macular hole needs more active treatments. Oncea central black blind spot is discovered in one eye, always consult a professional ophthalmologist as soon as possible.